Glaucoma, the silent thief of sight is the most common cause of irreversible blindness. Around 12 million people affected in India, of which 1.1 million are blind due to it.
Initially patients do not have any complaints but as it progresses detoriation in vision in noted, thus many patients present at later stage unless detected early by your ophthalmologist. Treatment options are aimed at preserving further loss of vision.
|
Commonly asked question by the patients is – “Is glaucoma curable?” Unfortunately glaucoma is not curable & causes irreversible blindness. Treatment options are aimed at preserving existing vision & prevent further loss of vision. Therefore it is important to detect & treat glaucoma early to preserve useful vision, just like diabetes mellitus & hypertension which require regular monitoring and lifelong follow up. |

TYPES OF GLAUCOMA
PRIMARY OPEN ANGLE GLAUCOMA
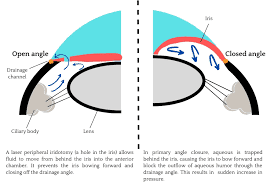
PRIMARY OPEN ANGLE GLAUCOMA – is the most common type of glaucoma. In this type of glaucoma, the fluid drainage channels of the eye is open, but there maybe defect leading to increased resistance to the outflow of fluid within the eye. In a few cases there maybe increased production of the fluid. This causes increased pressure within the eyeball. This develops slowly over time without any symptoms. Initially it affects the peripheral or side vision and very gradually progresses to the centre. This is the reason why many people are not aware that they have the condition until they have significant vision loss affecting central vision.
Risk factors for primary open angle glaucoma are :
- Age more than 40 years
- Family history of glaucoma
- Systemic diseases such as diabetes mellitus, hypertension, heart disease
- High myopia or those with a high minus power
- Race – African Americans
ANGLE CLOSURE GLAUCOMA OR CLOSED ANGLE GLAUCOMA
ANGLE CLOSURE GLAUCOMA OR CLOSED ANGLE GLAUCOMA – is the second most common type of glaucoma , in this form the drainage channels are narrow. Gradual closing of the angle is called chronic angle closure and if the drainage angle closes suddenly, it causes an acute angle closure attack. Acute angle closure glaucoma usually presents as an emergency. A patient who is in an acute angle closure attack will have symptoms of eye pain, redness, blurred vision, coloured halos, nausea and vomiting due to a rapid rise in the eye pressure.
You must see your ophthalmologist immediately.
Risk factors for angle closure glaucoma :
- Age more than 40 years
- Family history of glaucoma
- Women
- High hypermetropia or those with a high plus power
- Race – East Asians
NORMAL TENSION GLAUCOMA / LOW TENSION GLAUCOMA
NORMAL TENSION GLAUCOMA / LOW TENSION GLAUCOMA – In this type of glaucoma even though the pressure in the eye is normal the optic nerve can get affected. Although its cause is not entirely known or understood, it can occur either because of an extremely sensitive optic nerve that can get damaged even though the pressure in the eye is normal, or because of reduced blood flow to the optic nerve. As it is slow and silent people usually do not have any visual complaints until a very advanced stage of the disease.
Risk factors for normal tension glaucoma are :
- Family history of normal tension glaucoma
- Thinner corneas
- Heart disease
- Migraine and peripheral vascular disease
- Race – Japanese ancestry
CONGENITAL GLAUCOMA (CHILDHOOD GLAUCOMA)
CONGENITAL GLAUCOMA is rare but sight threating condition seen in infancy & childhood. This glaucoma is caused by abnormal drainage of fluid due to blocked or defective drainage channels (trabecular meshwork). Usually the child is brought for eye check up when the paediatrician or parents notice whitish discoloration, enlargement of the eyeball, sensitivity to light, excessive watering and tendency to keep the eyes closed. Treating congenital glaucoma in early stage can slow the development of the disease. Medical therapy and occasionally microsurgery can control the condition well in uncomplicated cases.
SECONDARY GLAUCOMA
There are certain other types of glaucoma where there is an identifiable cause for increased eye pressure resulting in optic nerve damage and vision loss, these are called secondary glaucoma. It may be caused by prolonged, indiscriminate use of steroids, severe diabetic retinopathy, injuries to the eye, inflammation of the eye (uveitis) or advanced cases of cataract.
PIGMENTARY GLAUCOMA
Pigmentary Glaucoma is a form of secondary open-angle glaucoma. It occurs when the pigment granules that are in the back of the iris (the coloured part of the eye) break into the clear fluid produced inside the eye. These tiny pigment granules flow toward the drainage canals in the eye and slowly clog them. This causes eye pressure to rise. Patients develop blurring of vision during exertion or exercise as more pigments are released. This kind of glaucoma is commonly seen in young, males with high minus power lenses (near sight).
TRAUMATIC GLAUCOMA
Injury to the eye may cause secondary open-angle glaucoma. Traumatic glaucoma can occur immediately after the injury or years later. It can be caused by blunt trauma that bruise the eye or by injuries that penetrate the eye. The elevated eye pressure following blunt trauma is temporary in most cases. However in some cases, the drainage canals in the eye can get damaged and permanently scarred. This scarring blocks fluid flow and can lead to glaucoma even several years after injury.
PSEUDOEXFOLIATIVE GLAUCOMA
In this form of secondary glaucoma a fleck, whitish grey dandruff like material peels off the outer layer of the lens. This material blocks the outflow drainage channels causing rise in eye pressure. This kind of glaucoma is more difficult to control with medical therapy and may require intervention.
NEOVASCULAR GLAUCOMA
Aggressive abnormal formation of new blood vessels on the iris and over the eye’s drainage channels can cause a form of secondary open-angle glaucoma.
Neovascular glaucoma is always associated with other abnormalities, most often uncontrolled diabetes and hypertension. It never occurs on its own. The new blood vessels block the eye’s fluid from exiting through the trabecular meshwork (the eye’s drainage canals), causing an increase in eye pressure. This type of glaucoma progresses rapidly and is very difficult to treat.
PATIENT CONSULTATION FLOW WHILE VISITING GLAUCOMA CLINIC AT AEH
What are the tests I need to undergo?
At 40, you should get your eyes examined & get a baseline optic nerve and pressure measured.
If you have risk factors for developing glaucoma like diabetes, high blood pressure, or a family history of glaucoma, you should see an eye doctor now to determine how often to have eye exams.
A comprehensive glaucoma evaluation includes the following tests which help in finding out the presence of glaucoma and also its progression in the subsequent follow-ups.
GLAUCOMA DIAGNOSTIC TESTS
|
Tonometry is a diagnostic test that measures the fluid pressure, known as intraocular pressure (IOP), inside your eye. |
Gonioscopy is a eye examination of the anterior chamber, to examine whether the area where fluid drains out of your eye (drainage angle) is open or closed. This test helps to differentiate between open or closed angle glaucoma and its line of management. |
The Visual Field test (Perimetry) It helps to plot and measure your peripheral or side vision (which is affected first by glaucoma), through which they can diagnose and monitor glaucoma. |
Ophthalmoscopy This examination helps the ophthalmologist to examine the optic nerve for glaucoma damage and its status. |
Apart from the above routine glaucoma tests, we may advice further investigations based on the type and severity of your glaucoma.
Aashirwad eye hospital is equipped with the most advanced diagnostic tools and investigational facilities needed to evaluate and diagnose common and rare forms of glaucoma.
All these new investigational modalities help us to detect the disease and progression early which aides us in better management of the patient.
- Intraocular pressure measurement ( Applanation tonometer, Avia Tonopen, non contact tonometer)
- Gonioscopy
- Ultrasonic Pachymeter
- Visual field analysis (Perimetry)
- Optical Coherence tomography (OCT)- Avanti
- Anterior segment swept source optical coherence tomography (Heidelberg engineering – Anterion)
- OCT angiography
- Ultrasound biomicroscopy
- Disc imaging- Optos ultrawide field retinal imaging system
GLAUCOMA TREATMENT OPTIONS
As the damage caused by glaucoma is not reversable, it is important to remain in regular check-ups so as to prevent vision loss. Glaucoma is treated by lowering your eye pressure (IOP-Intraocular Pressure). Depending on the stage of your disease, options may be eye drops, oral medications, laser treatment and surgery or a combination of any of these.
MEDICAL TREATMENT
Eyedrops are prescribed to lower the intraocular pressure either by improving fluid drainage or decreasing the amount of fluid production. Depending on the eye pressure you may require one or more eyedrops.
Some of these drops can cause mild irritation in the eyes, burning, redness or pigmentation. Rarely eye drops can also cause other side effects by getting absorbed systemically. Compliance to eyedrops is veery important to keep the progression in check.
LASER PERIPHERAL IRIDOTOMY (LPI)
Laser peripheral iridotomy is the standard treatment in angle closure glaucoma and eyes at risk for this condition. In this minor procedure, the Nd-yag laser beam creates a hole in the iris to an alternative pathway for the outflow of fluid.
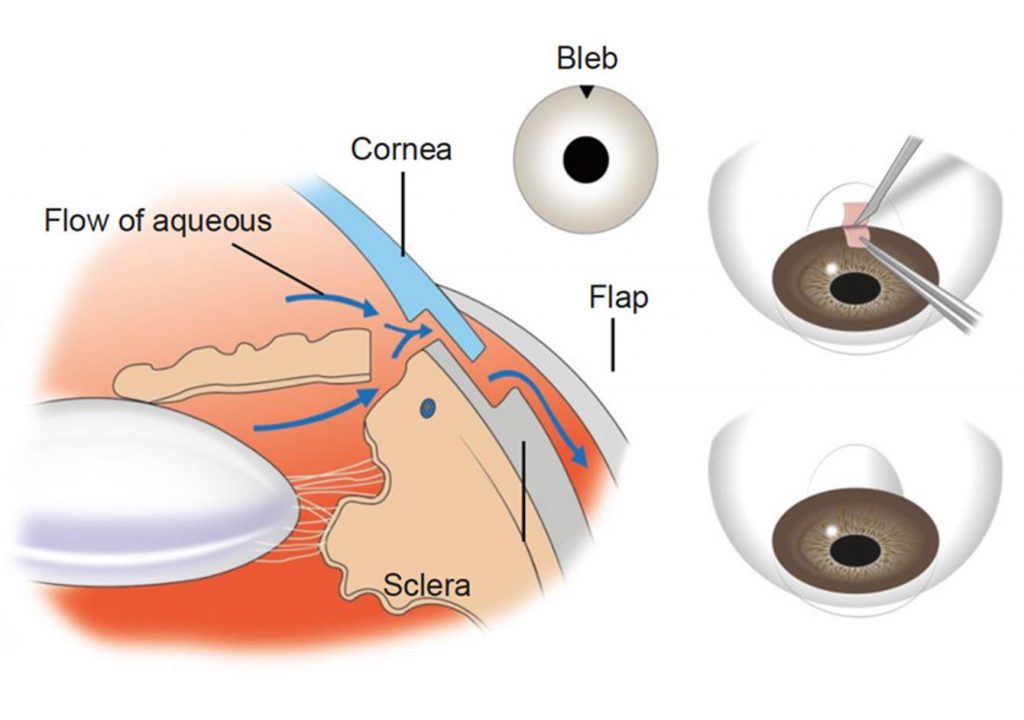
TRABECULECTOMY
It is a surgical procedure to lower the eye pressure when medical therapy or laser treatment has failed. A small window is made in the wall of the eye which is guarded by a flap that acts as a trap door. The fluid is shunted from inside the eye in a controlled fashion, which forms a small ‘bleb’ underneath the upper eyelid.
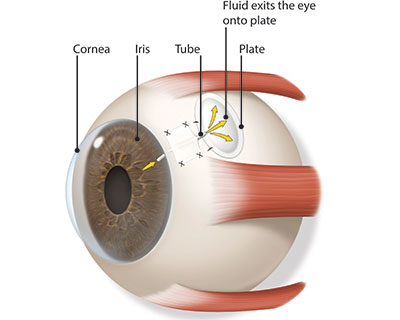
GLAUCOMA DRAINAGE DEVICE (GDD)
In certain cases of glaucoma tube shunt surgery may be required to divert aqueous humour (fluid inside the eye) from within the eye to an external reservoir.
Ahmed Glaucoma Valve (AGV) / Aurolab Aqueous Drainage Device (AADI) are the commonly used glaucoma drainage devices made of silicon polypropylene. It is shaped like a miniature computer mouse with a tube that enters the eye, while the rest of the implant sits on the surface of the eye, under the conjunctiva and is covered by the eyelid. Majority of the tube shunt procedures are successful and prevent progression to blindness that can occur with glaucoma.
TRANSSCLERAL CYCLOPHOTOCOAGULATION (TSCPC)
In this procedure diode laser is used to cause destruction of the ciliary body (structure which produces the clear fluid of the eye) and hence lower the eye pressure. This procedure is used severe refactory cases to prevent complete loss of the eye, usually in multiple failed glaucoma filtration surgeries or in case of a painful blind eye to provide relief. TSCPC is usually an effective and reasonably safe procedure.